A team of researchers hope to help the need for liver transplants with a successful animal-to-human transplant. The team connected a pig liver to a human to help create a “bridge to a transplant.”
Step in the right direction
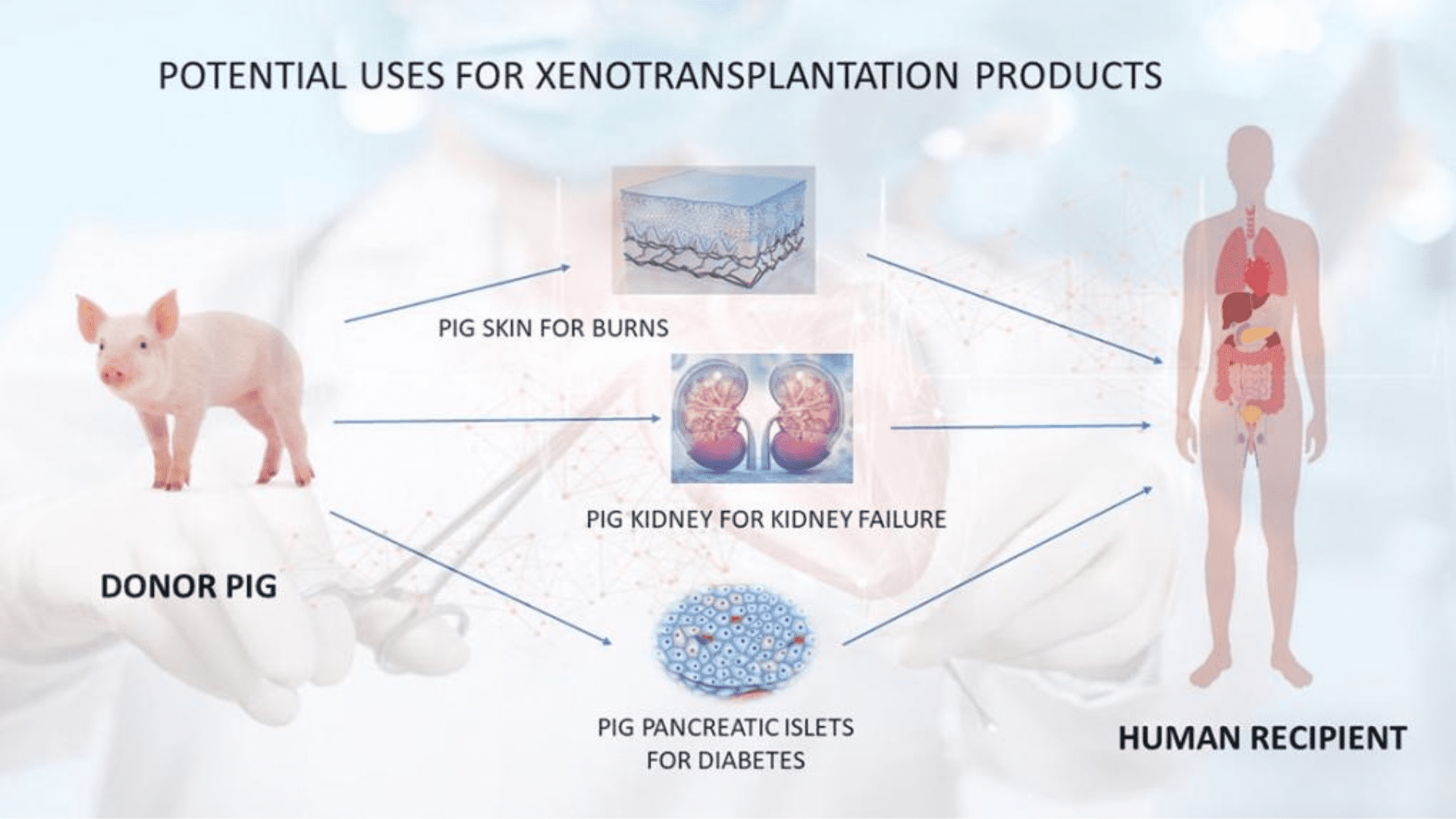
Researchers at the University of Pennsylvania are creating hope for patients waiting for a liver transplant. The team successfully filtered blood through a pig liver attached to a human body. Animals are a huge part of the medical world, especially in research. Animal-to-human transplants date back to 1966 when the first monkey-to-human transplant was carried out. Xenotransplantation is the name of the process. It’s a common practice for kidney transplants or skin grafts that use parts of a pig. A liver transplant using a pig liver is something of a marvel. For the first time ever, the University of Pennsylvania successfully did it in an experiment.
Researchers call it a “bridge-to-transplant.” The pig liver is not intended to stay in the human. But rather buy some time for the patients on the waiting list. In a statement form the University of Pennsylvania, they say, “across the country, more than 10,000 patients are waiting for liver transplants, and some patients run out of time waiting for a new organ.”
Explore Tomorrow's World from your inbox
Get the latest innovations shaping tomorrow’s world delivered to your inbox!
I understand that by providing my email address, I agree to receive emails from Tomorrow's World Today. I understand that I may opt out of receiving such communications at any time.
The study
It’s interesting how the researchers went about the study. Instead of putting the liver inside the human body, it stays outside and the researchers monitor how the liver works. It also gives them a better idea on how to treat a failing liver. It’s also important to discuss the patient in the experiment. A family donated the patients body because the organs were deemed unsuitable. The patient is brain dead and the team used a machine to circulate the blood through the pig liver and the body. For 72 hours, the patient remained stable and there were no signs of damage to the pig liver.
Again, the method is a bridge to a transplant. It is not meant to be a long-term treatment but more like a buffer for a patient on the transplant list. With the liver doing blood-cleansing work outside of the patients body, like what dialysis does for kidney failures. Because humans typically reject animal organs, researchers modified the pig liver to make it more “humanlike.” Genetically modified kidneys were used in temporary transplants in brain-dead patients to see how they function. Additionally,
Future studies
The Food and Drug Administration is considering to allow limited patients waiting for an organ to volunteer for studies to receive pig kidneys or hearts. For liver failure, transplants are the only cure at the time. Researchers at UPenn says, “unlike patients with heart or kidney failure, there are no mechanical options available to replace the functions of diseased livers prior to transplant.” According to the researchers, every year over 330,000 people need liver failure treatment in the United States.